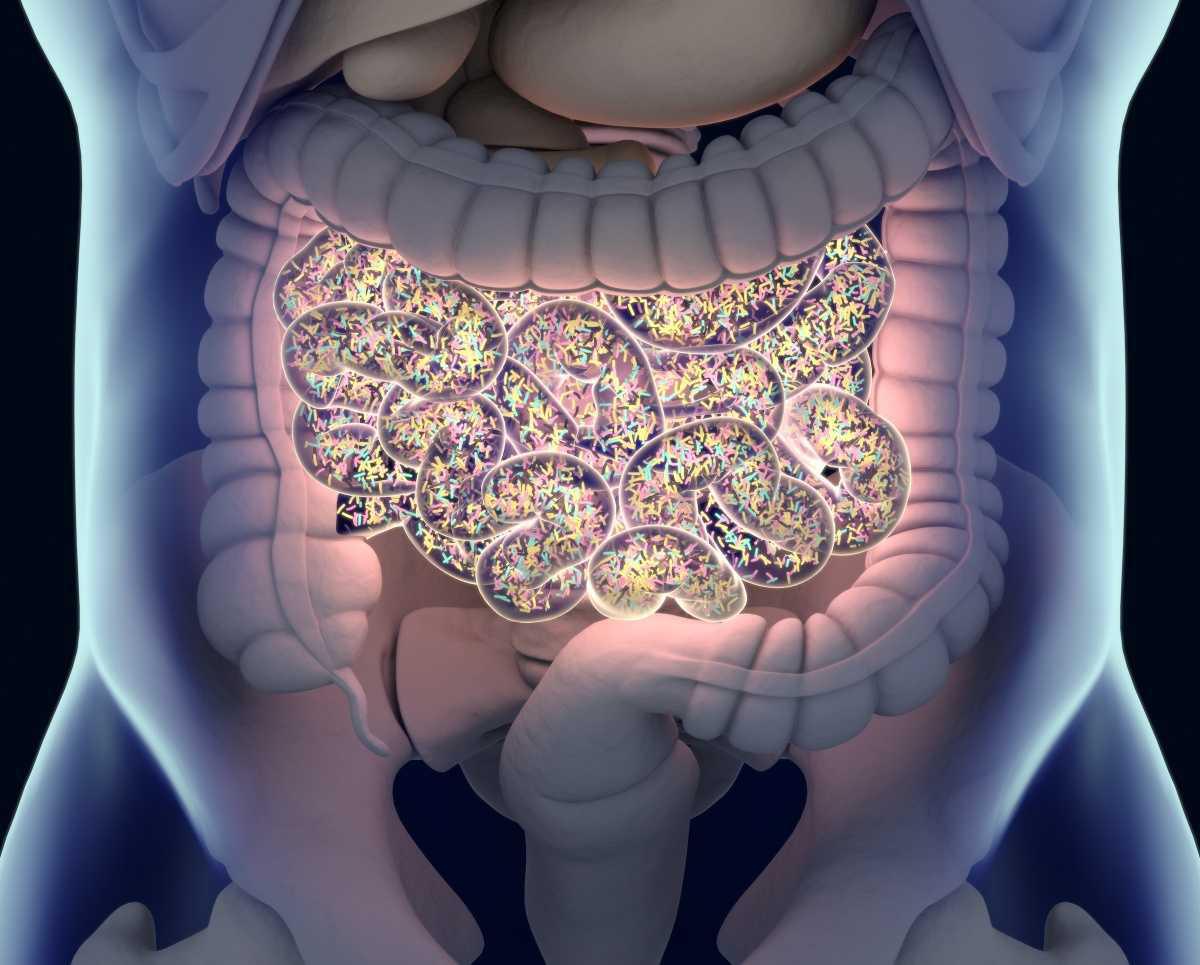
In recent years, scientific interest in the human microbiome—the trillions of microorganisms residing in our digestive tract—has exploded. Once dismissed as mere bystanders in digestion, these bacteria, viruses, and fungi are now recognized as major players in our overall health. Groundbreaking research continues to reveal that our gut microbiome influences everything from our immune system and metabolism to mental health and the risk of chronic diseases.
The Gut–Brain Axis: More Than a Metaphor
One of the most compelling findings in microbiome research is the strong link between gut health and mood regulation. This connection, known as the gut–brain axis, operates through a complex web of neural, hormonal, and immune signals. Certain gut bacteria produce neurotransmitters like serotonin, dopamine, and GABA, which directly affect brain function. In fact, up to 90% of serotonin is produced in the gut, suggesting that mental health is deeply intertwined with gastrointestinal well-being.
Studies have shown that people with depression and anxiety often have less microbial diversity and imbalances in specific bacterial strains. Probiotic interventions and dietary changes targeting gut health have shown promise in reducing symptoms of mood disorders—an emerging field known as psychobiotics.
Immunity Starts in the Gut
A robust immune system depends on a healthy gut. Around 70% of the body’s immune cells reside in the gut-associated lymphoid tissue (GALT), and the microbiome plays a critical role in training these cells to distinguish between friend and foe. Beneficial microbes help regulate inflammation, prevent autoimmune responses, and even increase the effectiveness of vaccines.
Imbalances in the gut microbiota, known as dysbiosis, have been linked to conditions such as allergies, asthma, and autoimmune diseases. Scientists are now exploring ways to harness the microbiome to boost immunity, especially in vulnerable populations.
Chronic Diseases and the Microbial Connection
Chronic diseases such as obesity, type 2 diabetes, cardiovascular disease, and even some cancers are increasingly being linked to disruptions in gut microbiota. These imbalances can influence insulin sensitivity, fat storage, and systemic inflammation—key factors in the development of long-term health issues.
One landmark study found that people with high levels of certain anti-inflammatory gut bacteria had a significantly lower risk of developing heart disease. Another study linked specific microbial profiles to longevity, suggesting that gut health may be a biomarker—and perhaps even a driver—of healthy aging.
What You Can Do for Your Gut
Thankfully, supporting your microbiome doesn’t require a medical degree. Here are a few science-backed steps you can take:
-
Eat a diverse, fiber-rich diet: Whole grains, legumes, fruits, and vegetables feed beneficial bacteria.
-
Incorporate fermented foods: Yogurt, kefir, kimchi, and sauerkraut are rich in probiotics.
-
Avoid overuse of antibiotics: While sometimes necessary, antibiotics can wipe out beneficial microbes.
-
Manage stress: Chronic stress can negatively impact the gut–brain axis.
The Future of Gut Health
Microbiome research is still in its early stages, but it’s already reshaping how we view health and disease. Personalized probiotics, microbiota transplants, and gut-based diagnostics are just some of the innovations on the horizon. As scientists continue to decode the secrets of the microbiome, one thing is clear: taking care of your gut is no longer just about digestion—it's a cornerstone of whole-body wellness.